San Antonio Uniformed Services Health Education Consortium
History of the Wilford Hall USAF Allergy/Immunology Training Program
The Allergy Program was approved by the Certifying Committee in 1962. Robert E. Smith, a pediatric/allergist, trained at Scripps Clinic in California, was the first Chief. He was assigned to the Department of Pediatrics in 1957 and functioned within that department as he initiated efforts to establish an Allergy Training Program. This was particularly difficult for the program would have to be a section within the Department of Internal Medicine. After approval of the program, space had to be allocated and staffing had to be obtained to operate a clinic. The clinic was located on the first floor of Wilford Hall Medical Center until 1970 when it was moved to one of the wards from the old, WWII Lackland AFB Hospital. The clinic was moved back into the newly constructed out-patient addition to the main hospital in 1980.

Initiation of the Fellowship Program; 1964
In July, 1964, the first fellow, Andrew M. Hegre, an internist, came into the program. Smith and James Tannenbaum were the only staff.
In July, 1965, additions were made to the staff including Stephen R. Shapiro, an internist trained in allergy at Walter Reed, and J. Terence Sams, an internist, trained in allergy for one year at Ohio State and then drafted into the military. Max I. Michels, a pediatrician from the field, joined Andrew Hegre as fellows.
In July1966, James Tannenbaum returned to Ohio State as a staff physician and Andrew Hegre took an assignment and, after his military commitment , began his practice in New Orleans. The staff slot vacated by Tannenbaum was unfilled. Another fellow, Ramon Casanova-Roig, a pediatrician, joined second-year fellow, Max Michels.
In July, 1967, Robert Smith moved into an administrative position and Terence Sams exited the military and started a practice in Arlington, Texas. Max Michels was elevated to Chief of the allergy program despite just finishing his fellowship. This created some discord between him and Stephen Shapiro. Michels was superior in military rank but inferior to Shapiro in experience. No new staff and no new fellows were added to the program.
In 1968-69, Michels and Shapiro were the only staff and no fellows were in the program. Ramon Casanove-Roig had taken an assignment to the field and later began a practice in Puerto Rico.
In July, 1969, Eugene S. Lebauer (University of Colorado) was a new added staff. A fellow was accepted: Aubrey M. Worrell, a pediatrician. The clinic was moved from the main hospital to an old ward of the Lackland hospital (World War II style building). This building was large enough to house a few staff and fellows but proved inadequate as the program grew during the late 1970s.

In 1970, the staff remained unchanged, however, another fellow, H. Norman Richardson joined Aubrey Worrell as a second fellow. No research was ongoing and no meaningful publications were done.
In July, 1971, Lebauer separated and joined his father’s practice in Greensboro, NC. A new staff, John R. Bozalis, an internist trained in allergy at University of Michigan, was added. A new fellow, Robert L. Jacobs, joined Richardson as the 1st year fellow. Worrell took an assignment and later started practice in Arkansas. Bozalis was instrumental in the drive to improve the program by pointing out that there was no research being done and there were no laboratory capabilities available. He also brought in a somewhat different perspective and personality. He was more involved in teaching, not only of the fellows but the internal medicine residents. He also led a push on the Department of Medicine to allow hospital admitting privileges for the allergy staff and fellows.
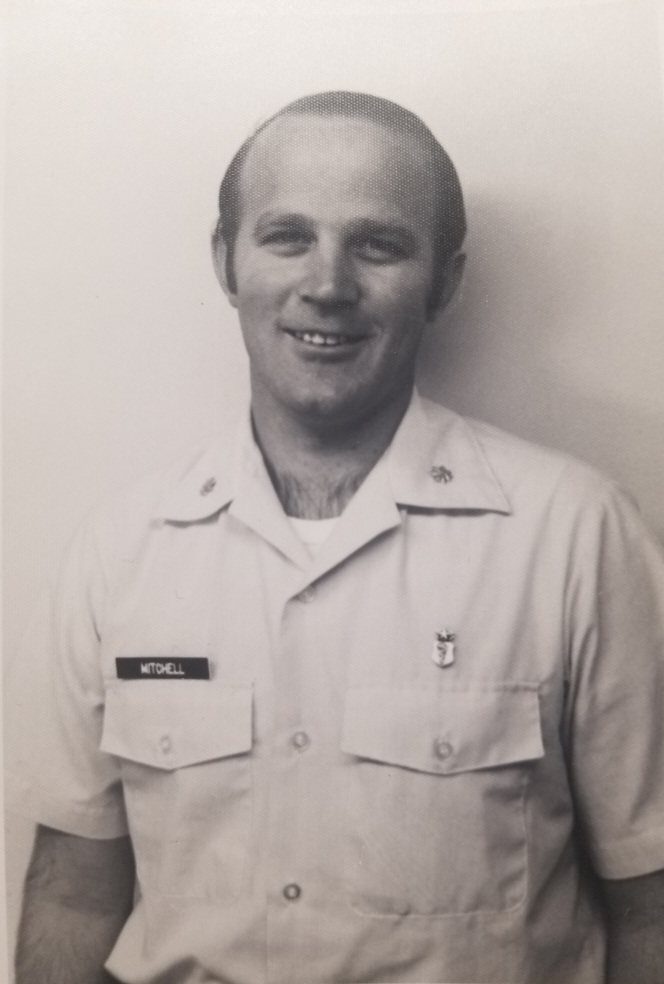
1972 brought a new staff, Stacey Greenert, an internist trained in allergy at Cincinnati, and a 1st year fellow, Don Q. Mitchell, an internist (Who would later become a President of the American College of Allergy, Asthma and Immunology). Richardson departed and, after retirement from the USAF, started practice in California. Greenert had a photographic memory and could quote the page number of a text where one could find a piece of information. Because of his unique personality, he was the source of many unusual stories that are talked about today by those individuals who knew him. He started practice in Cincinnati upon separating from the USAF.
In July, 1973, Stephen Shapiro took an assignment to Germany. Bozalis separated and began practice in Oklahoma. Jacobs was retained on the staff and was joined by Joseph F. Kelly, an internist, trained in allergy at Northwestern in Chicago. Joseph Kelly had trained under Roy Patterson (who had served as the National Consultant in Allergy/Immunology for the USAF) Kelly, like Bozalis, also brought a somewhat different perspective to the program. Edwin O. McCluskey, an internist, became a 1st year fellow with his second year to be served in Rheumatology in Denver. Don Q. Mitchell moved into his second year of fellowship.
In July, 1974, Max Michels retired and Stacey Greenert separated. Jacobs was elevated to Chairman and Director of the Training program. However, because allergy boards were given every other year, Jacobs had not taken boards and the program was discontinued. R. Neal Boswell, an internist, was assigned to the staff, however, he had no formal allergy training (There was a shortage of trained allergist in the military). Don Q. Mitchell was retained on the staff and Edwin McCluskey took an assignment since his Denver fellowship in Rheumatology had fallen apart. Bobby Q. Lanier (who would later become a President of the American College of Allergy, Asthma, and Immunology) transferred from the program at Galveston and spent the last 6 months (Jan – Jul 1974) of his fellowship at Wilford Hall. Notable in 1974, Jacobs and Mitchell began research projects in collaboration with the army allergists at Ft. Sam Houston leading to two classic papers published in the same edition of the Journal of Allergy and Clinical Immunology related to Immunotherapy to Fire Ants and to Mountain Cedar pollen. The Wilford Hall IRB, at that time, was controlled by an individual who felt that any research to be approved needed to be of “Noble Prize” importance, making it very difficult to do any research at Wilford Hall.
In July, 1975, Jacobs added Lanier and Peter M. Freedmen to the staff. Boswell was sent to Harvard to study bench-type immunology in order to return to boost the scientific side of the program. Mitchell separated from the USAF and started practice in Jackson, Mississippi. Freedman, an internist, had trained at Scripps Clinic and was academically inclined. No fellows were taken. Jacobs passed boards in October 1975 and immediately began to re-activate the training program. Since Lanier had spent ¾ of his training in an academic program, he was assigned to draft the outline of the Allergy/Immunology Program that we would begin at Wilford Hall in 1976. Freedman was assigned to confiscate any usable equipment from the massive warehouse storage areas at Kelly AFB and begin to build a functioning laboratory. Plans were being drafted to design and build onto Wilford Hall. Jacobs began to plan for an appropriate clinical facility with a significant laboratory space for the Allergy/Immunology Department. The protocol to study and define the NARES patients was developed and written by Jacobs and Freedman. Collection of data for the Tetanus Toxoid paper was started. Despite these ongoing efforts, we had to manage the clinic patients with a reduced staff (Jacobs, Lanier, and Freedman) and no fellows.
In the spring of 1976, the Accreditation Committee accepted our Training Program plan in time to accept two fellows, Normand F. Tremblay, a pediatrician, and Ralph S. Lowe, an internist. W. Cleve Posey, a pediatrician, trained in allergy at Fitzsimmons in Denver joined the staff. The training program plan generated primarily by Lanier was adopted as the model for other training programs, however, no credit was ever given to Bobby Q. Lanier. Lanier went into practice in Fort Worth in July 1976. Peter Freedman extended for a year until July 1978.
This was the year, 1976, in which the NARES and Tetanus Toxoid studies were initiated. The first patient that had severe anaphylaxis while on beta-blockers was seen in the hospital referred from Sheppard AFB in North Texas. The anaphylaxis patient was of high interest with Freedman pointing out that the pattern was consistent with what one would see with beta-blockade. This was not published until a 2nd case was seen in 1980.
In July 1977, Boswell returns from Harvard and becomes involved with the NARES protocol adding a nasal wash to increase the scientific value of the study; Freedman continues to run the laboratory; Jacobs and Posey continue on staff; Tremblay and Lowe continue as 2nd year fellows; Robert E. Harvey and Donald Fournier came on board as 1st year fellows.
1979: Tremblay separates and joins Lanier in practice in Fort Worth; Harvey and Fournier remain on staff for one year before going into field; Guillermo Villacorte, from Creighton Medical College, joins staff to boost the laboratory capabilities; Two new fellows: Jimmy Chevalier and Bruce L. Nelson join Strom, Culver, and Sacha; Angelo J. Freda transfers from Florida as a second year fellow; plans for new facilities in WHMC finalized; Jacobs and Boswell presented the NARES paper in New Orleans at AAAAI meeting. In the spring of 1980, potentiated anaphylaxis occurred in a patient following an immunotherapy injection in the old clinic building. Bill Culver, Don Fournier, and the cardiology staff spent hours before stabilizing the patient. I had seen the prior patient, three years earlier, referred from Sheppard AFB after the event, but did not recall the name nor did I have any records. Don Fournier spent a month searching the patient records who had been admitted to WHMC during this time period before finding the records.
The NARES Presentation
There were two USAF NARES abstracts presented: one by Bob Jacobs and the other by Neal Boswell. Their abstracts immediately followed the abstract from the Mason Clinic by Mike Mullarky on the same subject. These presentations were considered revolutionary at that time because all chronic rhinitis problems were felt to be of allergic causation and the A/I problem was that we did not test to the correct allergen. This picture was taken after the presentation when Dr. Jacobs had answered a question concerning foods as the allergic cause for NARES. He had replied that they did not believe that foods caused allergic rhinitis except during a systemic reaction which created an uproar from the pediatricians in the audience. The paper had been submitted as two papers, and after prolonged reviews, the data was accepted but required to be combined into one paper. There was a delay among the authors in combining the papers. That is the reason that Mullarky published his paper a year before Wilford Hall published. The Wilford Hall paper became the dominant publication, not because of the content, but because of the name: NARES. Reference: Jacobs RL, Freedman PM, Boswell RN. Nonallergic rhinitis with eosinophilia (NARES syndrome). J Allergy Clin ImmunoI 1981;67:253-62

In July, 1980, Fournier , Sacha, Freda, and Harvey go into the field; Culver and Strom remain on staff; Three new fellows come aboard: James Claflin, Geoffery W. Rake, and Dexter DeWitt; Moved into new facility in the new WHMC addition; Had to give up about 2/5th of our new space to the Dermatology section because they had made no plans for the new facility; Acquired a new position for a Laboratory Technician to manage the laboratory; Acquired a Personal Secretary (Annie Holmes); Presented and published the “Potentiated Anaphylaxis” paper and published the NARES paper in JACI in the spring of 1981.
In July 1981: Nelson and Chevalier go to the field; Three new fellows come aboard: Jeffery S. Hallett, Gregory K. Lux, and Edwin J. Whitney; DeWitt was dismissed from training; Staff remains the same; Published Tetanus paper in JAMA which was translated into German, Japanese, and Russian for JAMA publications in those countries; several other publications were accomplished in 1982;
In July,1982: Claflin and Rake go to the field; Whitney withdraws from the program and enters a cardiology fellowship; Two new fellows arrive, Gary L. Smith and Arthur N. Fokakis; Staff addition of Bruce Martin from Fitzsimmons AMC; Boswell transferred to an Immunology laboratory set up by Jacobs and Robert Lordon (Chairman of Medicine) to manage the influx of patients with what would be known as AIDS later; Acquired a position for a fellow to do a third year of Laboratory Immunology at a civilian facility;
In July1983: Hallett and Lux go to the field; Lux was turned down for the third year of immunology training on the basis that he had the military pay for college (Air Force Academy), medical school, pediatric residency, and fellowship (13 years) and he had never served in the field; Three new fellows came aboard: Raiqua Arastu, Luis Matos, and Edward E. Philpot; Strom separates and goes into practice in Paris, Texas; Culver takes an assignment to Wiesbaden, Germany with the plan to return and take over as Chairman when Jacobs retires in 1986; Michael Ruff joins the staff from Duke; Six year rule was to be enforced leading to disruption of plans; Jacobs forced to retire in June 1984; Search for a new chairman began and ended with Bruce Martin elevated to that positon in July, 1984.
SUMMARY: The first 8 years was clearly only a clinical allergy program. There was little known science, as compared to the present time, and there was a lack of proper laboratory facilities. The only equipment in the clinic was a spirometer and a slide-staining tray (for doing nasal and sputum smears). Robert Smith continued to publish but no sustained research efforts were undertaken by Michels and Shapiro.
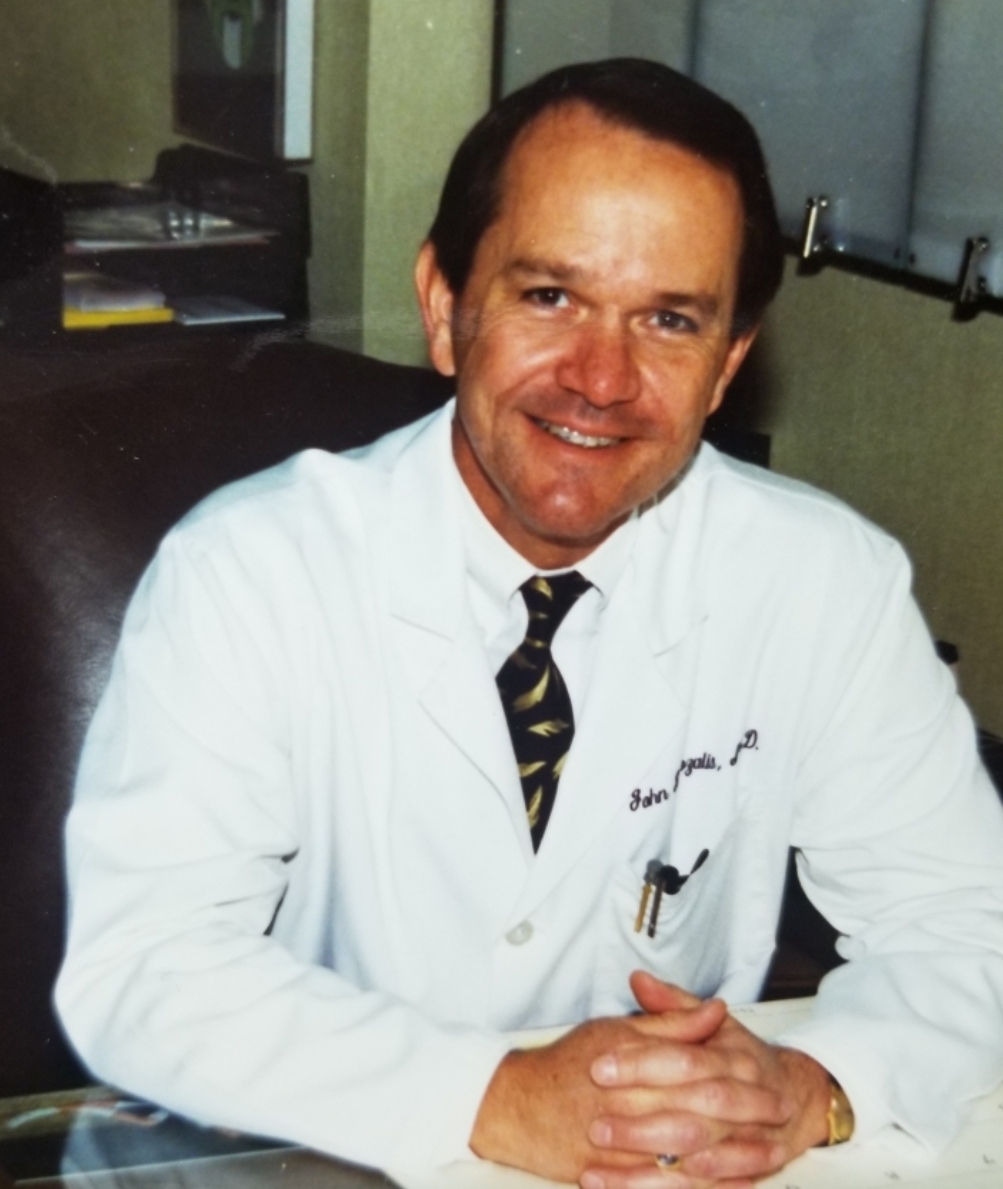
In the second 10 years, dramatic changes occurred. Six individuals played significant roles in the development of the Allergy/Immunology Program as it now functions. Three staff, who did not overlap, contributed to a change in attitude concerning the allergy/immunology approach: John R. Bozalis 71-73 (Michigan trained) and Joe F. Kelly 73-75 (Northwestern trained) were both amazed at the number of patients and pathology seen at Wilford Hall and recognized the potential for meaningful research. Peter M. Freedman 75-78 (Scripps Clinic) was instrumental in developing the 1st laboratory and was an intellectual power on the teaching side.
To begin the transition to a different approach, Mitchell and Jacobs conspired with the army allergist at Brook Army Medical Center to do two studies. Bobby Q. Lanier drafted the format for modern combined allergy/immunology programs as we activated the Wilford Hall program. This format was adopted by the Certifying Board for Allergy/Immunology training programs and remains the standard for which all allergy-immunology training programs must meet to remain certified. Peter M. Freedman developed a laboratory, using equipment from the warehouses at Kelly AFB, to lay the foundation for a more sophisticated laboratory in the planned new facilities. Robert L. Jacobs developed the plans for the new facilities. R. Neal Boswell was granted a fellowship at Harvard to develop and manage the more sophisticated laboratory.
The initial research efforts took place with army allergists at Brooke Army Medical Center (due to difficulty with IRB approval at Wilford Hall) leading to two hallmark papers concerning immunotherapy to Mt. Cedar allergy and Fire ant allergy. Research protocols were begun on Tetanus Toxoid sensitivity and NARES syndrome. Two patients with anaphylaxis potentiated by propranolol were recognized. These three papers were highly recognized world-wide which cast the program at Wilford Hall as one of the top programs in the country. (Our program was in direct competition with the Fitzsimmons Army Allergy/Immunology program directed by Harold Nelson for the top programs)
Upon moving into the new facility in 1980, the program continued to flourish. The facility was very spacious allowing office space for all fellows, adequate laboratory area, and a conference room. Bert Strom remained on the staff and completed the first study utilizing the new laboratory area. This protocol required ‘milking’ of live fire ants to collect venom. This fire ant paper confirmed a previous paper with objective data and set the stage for several additional studies by future staff and fellows concerning fire ants. A paper concerning primary nasal polyps coupled with the NARES paper and a publication from Mason Clinic in Seattle were credited with cleaving nasal disease into allergic and non-allergic forms.
In 1982, because of a high level of referrals for an acquired immune deficiency in homosexuals, Jacobs and Robert Lordon (Chairman of Department of Medicine) assigned an allergy staff slot and R. Neal Boswell with developing an Immunology Laboratory to manage this population.
In 1983-84, the six-year rule was enforced that disrupted individual allergists careers but did not disrupt the trajectory of the training program.
Robert L. Jacobs retired in 1984 and Bruce G. Martin assumed the Chairmanship.
The Six-Year Rule
A Six-year rule was enforced beginning in 1983-84 that required assignment of all personnel who had been on a station for 6 years to be transferred to another facility. This rule had not been utilized in the past.
Background: This was a political move, instigated by the newly appointed Surgeon General, to punish the “cronies” at Wilford Hall of the former Surgeon General, Paul Meyers. Meyers had spent 22 consecutive years at Wilford Hall Medical Center, moving up in rank to Major General, before being appointed to the Surgeon General slot (which had always been a three year assignment). Meyers was very effective at this position and was given a 4th year, which infuriated the Major General who was expecting to be elevated to that position. This Major General had been a flight surgeon and knew high-ranking line officers, who he was able to convince that many of the physicians at Wilford Hall were not of the highest caliber and were kept there because of friendship with General Meyers. They were to be rotated into the field with physicians at other medical centers brought to Wilford Hall to replace them. This Surgeon General had little perspective as to what it took to run a training program.
Result: Robert L. Jacobs and Robert A. deLemos had been on station at Wilford Hall for 15 consecutive years and were made “scapegoats” as individuals who had abused the system by various nefarious methods to remain at WHMC for such a prolonged period. We were summoned to Randolph AFB and told that we were being re-assigned across 2 military zones to prevent an “insurrection”. Jacobs was to be re-assigned to Travis AFB and deLemos was to be re-assigned to the Phillipines. Jacobs was forced to retire, however, deLemos had only 18 years military service. In a masterful (nefarious ?) strategic move, deLemos applied for retirement, post-dated to the point of 20 years service and, therefore, he could not be re-assigned. This further infuriated the Surgeon General.
The effect on individual allergist in the USAF was significant. Culver would not be allowed to return to be Chief; Bruce Martin was also forced to separate or take an assignment within another2 years; Mike Martin was assigned to WHMC from Malcolm Grow Medical Center; Mike Reid was forced to move from Travis to WHMC; Villacorte was forced to separate. There was little to no effect on the program. The staff and fellows performed at a high level as expected.
This enforcement of the six-year rule was reversed by the next Surgeon General as it was recognized as a massive mistake that had much more serious consequences for other departments. This reversal allowed Ted Freeman to become Chief and to serve in that position for 13 years, Dave Goetz to remain on staff for more than 10 years, and Jim Quinn to serve in the capacity of staff and then Chief for several years beyond the six-year limit. Those that had been directly affected have been very successful and all ended up in the areas that they probably would have gone to without an interruption by the six-year rule.
Robert A. deLemos was at WHMC from 1969 to 1986. He was not directly associated with the Allergy/Immunology Department but his residents played critical roles in caring for hospitalized asthmatics during the periods when the allergy/immunology staff was short-handed. This obituary outlines his career revealing his importance to the history of Wilford Hall and the Allergy/Immunology Program.
Bob deLemos had a distinguished, if far too brief, medical career focused on the care of premature infants with lung problems.
At Amherst he was a Bond Fifteen history major who became premed only in junior year. After Amherst he received his MD cum laude from Harvard Medical School in 1962, followed by an internship and residency at Children’s Hospital in Boston, and a fellowship in neonatology at Johns Hopkins Medical Center. There he worked with Mary Ellen Avery, an early pioneer in the new field of neonatology.

Bob’s interest in premature infants was fueled by the death of John F. Kennedy’s infant son, who died from hyaline membrane disease while Bob was a pediatric resident at Children’s. Much of his very successful 30-year research career focused on the search for treatments for this disorder and related complications.
He played a critical role in the development of a new high-frequency ventilator for premature infants with injured and poorly developed lungs (a respirator that classmate-physician Al Most called “revolutionary”). This advance contributed to the remarkable improvement in survival that has occurred for premature infants over the past four decades.
Bob was the chairman of pediatrics at Wilford Hall Hospital at Lackland Air Force Base in San Antonio. After retiring from the Air Force as a full colonel, he was the chairman of the Department of Physiology and Research at the Southwest Foundation for Biomedical Research in San Antonio.

In 1991 he moved to California and became Chief of Neonatology at the University of Southern California in Los Angeles, and Hastings Professor of Pediatrics and director of neonatal intensive care at Good Samaritan Hospital. He was also a consultant to the Surgeon General of the U.S. Air Force.
His academic career was characterized by tremendous commitment to the care of the babies and their families who needed him, as well as a true passion for teaching and research. He was one of the first and most influential neonatologists in this country, and he taught many fine men and women who were inspired by his passion, knowledge, and understanding to dedicate themselves to medicine and to the specialties of pediatrics and neonatology.
But Bob is fondly remembered as much for his community service as for his clinical and research work. He served as team physician when his older sons, Steven, James and David played football from Junior League, through Middle School and High School. Dr. “D,” as Bob was called, was respected and loved by the players, the coaching staff, and the administration at the New Braunfels schools where he served.
Bob’s parents ran a camp in New York throughout his childhood. It is quite fitting that his passion in adulthood was a camp for disabled children near San Antonio, called Children’s Association for Maximum Potential (CAMP). Bob was a founding board member and served as president for 17 years. Moreover, he spent essentially all of his vacation time for many years at CAMP, even after he moved to Los Angeles. He made it his mission to give these kids a true camp experience regardless of whatever disability the child might have, and most importantly to have fun and to be treated with dignity and respect.
Al Most wrote in his “In Memory” sketch that Bob was a quiet man who never tooted his own horn. Yet after his death the San Antonio Express needed two long columns to document his caring for kids with special health needs. The local United Way created the “Bob de Lemos Volunteer of the Year” award to recognize a student who had logged the most voluntary service hours.
Bob’s enthusiasm for learning and education, his hard-core work ethic and a lifelong commitment to public service served as an example to his children. They have followed in his footsteps and have pursued professional careers in law, medicine, counseling and teaching, as well as involvement in a wide variety of good causes.
Bob has been missed by his family (including his sister, Anne, who is Bill Krupman’s wife) and friends, the countless patients and families he helped both directly and through his research, and the children and their families that he helped and touched through CAMP.
Robert A. deLemos died of a cerebral hemorrhage in Los Angeles Nov. 19, 1997.